Pelvic Pain, Bloating, and Backache? It Might Be Chronic Pelvic Pain Syndrome
Pelvic Pain, Bloating, and Backache? It Might Be Chronic Pelvic Pain Syndrome
Lower abdominal pain is a common issue among women.
However, if the discomfort becomes long-lasting and is accompanied by bloating, pressure, or lower back pain, it could be a sign of an underlying pelvic condition.
Pelvic pain—whether dull, aching, or cramping—is frequently reported among women aged 15 to 44. The causes can vary widely, ranging from normal physiological changes like menstruation and ovulation, to more serious conditions such as infections or endometriosis.
In this article, we’ll explore the causes and symptoms of pelvic pain and share ways to relieve discomfort— so you can reclaim a healthy, comfortable life.
Quick Overview of Pelvic Pain Syndrome
Pelvic Inflammatory Disease and Bloating — Warning Signs You Shouldn’t Ignore
Pelvic Inflammatory Disease (PID) is a common gynecological condition. In addition to lower abdominal pain and lower back discomfort, it may also cause bloating and other troubling symptoms. Recognizing these signs early can help ensure timely diagnosis and treatment.
Common Symptoms of PID
- Persistent Abdominal Pain: Ongoing discomfort in the lower abdomen, often dull at first and possibly spreading to the opposite side over time.
- Pain During Intercourse: Discomfort during sex, typically more noticeable during active inflammation.
- Abdominal Bloating: A sense of fullness, gas, or pressure in the stomach area.
- Increased Vaginal Discharge: More discharge than usual, possibly with an unusual odor.
- Menstrual Irregularities: Irregular periods or delayed menstruation.
- Fever and Systemic Symptoms: May include high fever, chills, headache, or general malaise.
- Gastrointestinal Symptoms: Such as nausea, vomiting, poor appetite, or diarrhea.
- Urinary Symptoms: Frequent urination or pain while urinating.
Get Expert Cardiovascular Advice Now
Expert Surgeons for Comprehensive Cardiovascular Treatment!
Instant Online Consultation Available
What Causes Pelvic Inflammatory Disease? 5 Common Risk Factors
1.Bacterial Infections
Bacteria such as Chlamydia trachomatis, Neisseria gonorrhoeae, or Escherichia coli can enter through the cervix—often via sexual activity—and spread upward to the uterus and pelvic organs.
2.Sexual Activity
Having frequent sex, initiating sexual activity at an early age, or having multiple sexual partners increases the risk of infection.
3.Poor Hygiene Habits
Inadequate hygiene during menstruation or excessive vaginal douching can disrupt the vagina’s natural defense system, making infections more likely.
4.Weakened Immunity
Low immunity due to fatigue, illness, or chronic health conditions can raise the risk of developing PID.
5.Contraceptive Devices
Using an intrauterine device (IUD) without proper sterile technique can allow bacteria to enter the uterus, increasing the chance of infection.
Will Pelvic Pain Go Away? Understanding Chronic Pelvic Pain Syndrome
Many women experience pelvic discomfort from time to time, but if the pain lasts for more than six months, it may be a sign of Chronic Pelvic Pain Syndrome (CPPS)—a condition that requires medical evaluation and treatment.
Pain associated with CPPS can affect the pelvic region, lower abdomen, lower back, buttocks, or inner thighs, and may interfere with urination, bowel movements, or sexual activity.
If left untreated, chronic pelvic pain may lead to the following complications:
➤ Worsening or Persistent Pain
Without treatment, pelvic pain may become more intense and long-lasting, affecting daily life and work. The pain can spread or worsen with movement.
Sexual Health Issues
Chronic pelvic pain often causes pain during intercourse, significantly impacting sexual well-being and possibly leading to emotional distance or relationship strain.
➤ Infertility or Difficulty Conceiving
When left untreated, chronic pelvic pain syndrome may affect reproductive health and increase the risk of infertility.
➤ Mental Health Challenges
Persistent pain can lead to low mood, anxiety, or depression, reducing overall quality of life. This can create a vicious cycle, where emotional distress intensifies the perception of pain.
Get Expert Cardiovascular Advice Now
Expert Surgeons for Comprehensive Cardiovascular Treatment!
Instant Online Consultation Available
How Is Pelvic Inflammatory Disease Treated?
If you experience symptoms such as lower back pain and abdominal bloating due to pelvic inflammation, it's important to seek medical attention promptly.
A gynecologist will conduct a thorough medical history review, physical examination, and necessary tests—such as ultrasound or blood work—to determine the cause and develop an appropriate treatment plan.
Treatment Options for PID
- Oral Antibiotics: For milder cases, doctors typically prescribe oral antibiotics to reduce inflammation and symptoms. The treatment course usually lasts 1 to 2 weeks.
- At-Home Heat Therapy: Patients with mild inflammation may use heat packs at home to relieve discomfort, relax muscles, and ease pain.
- Intravenous Antibiotics: For more severe symptoms, hospitalization with IV antibiotics may be necessary to better control the infection.
- Anti-Inflammatory Pain Relief: Non-steroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and discomfort.
- Surgical Intervention: If the infection worsens and leads to complications such as a ruptured tubo-ovarian abscess, emergency surgery may be required to remove the pus and prevent further spread.
Popular Questions About PID Symptoms
Q1. Is pain on the side of the pelvis a sign of Chronic Pelvic Pain Syndrome (CPPS)?
Pain near the pelvic area is not always CPPS, but if the discomfort lasts for more than six months and is accompanied by other symptoms—such as worsened menstrual pain, pain during sex, or difficulty urinating—it could be a sign of CPPS.
The following self-check is not a medical diagnosis but may help you understand when to seek care. If you have symptoms, it's best to consult a gynecologist as soon as possible.
- Duration of pain: Has the pain lasted for more than six months without significant relief?
- Type of pain: Is the pain dull, cramping, or stabbing?
- Location of pain: Is the pain limited to one specific area or does it spread elsewhere?
- Associated symptoms: Are there other symptoms such as fever, unusual vaginal discharge, or difficulty urinating?
Q2. Which areas can pelvic pain affect?
Pelvic pain can affect a wide range of areas. It often begins in the lower abdomen and may radiate outward to the lower back, sides of the pelvis, and even the inner or outer thighs.
During pelvic inflammation, the pain may feel deep, dull, or bloated in the lower abdomen, or like a pulling or dragging sensation. This discomfort can worsen with certain movements or positions, such as standing, walking, or during sexual activity.
In some cases, the pain may also spread to the lower back, causing backaches, or extend to both sides of the pelvis—near the hip joints—mimicking hip pain.
Q3. If I have bleeding and fever with suspected pelvic inflammation, which doctor should I see?
If pelvic inflammatory symptoms are accompanied by bleeding and fever, it’s important to visit a gynecologist as soon as possible.
In severe cases, hospitalization or even surgery may be required. Early medical attention is crucial for controlling the infection and preventing complications.
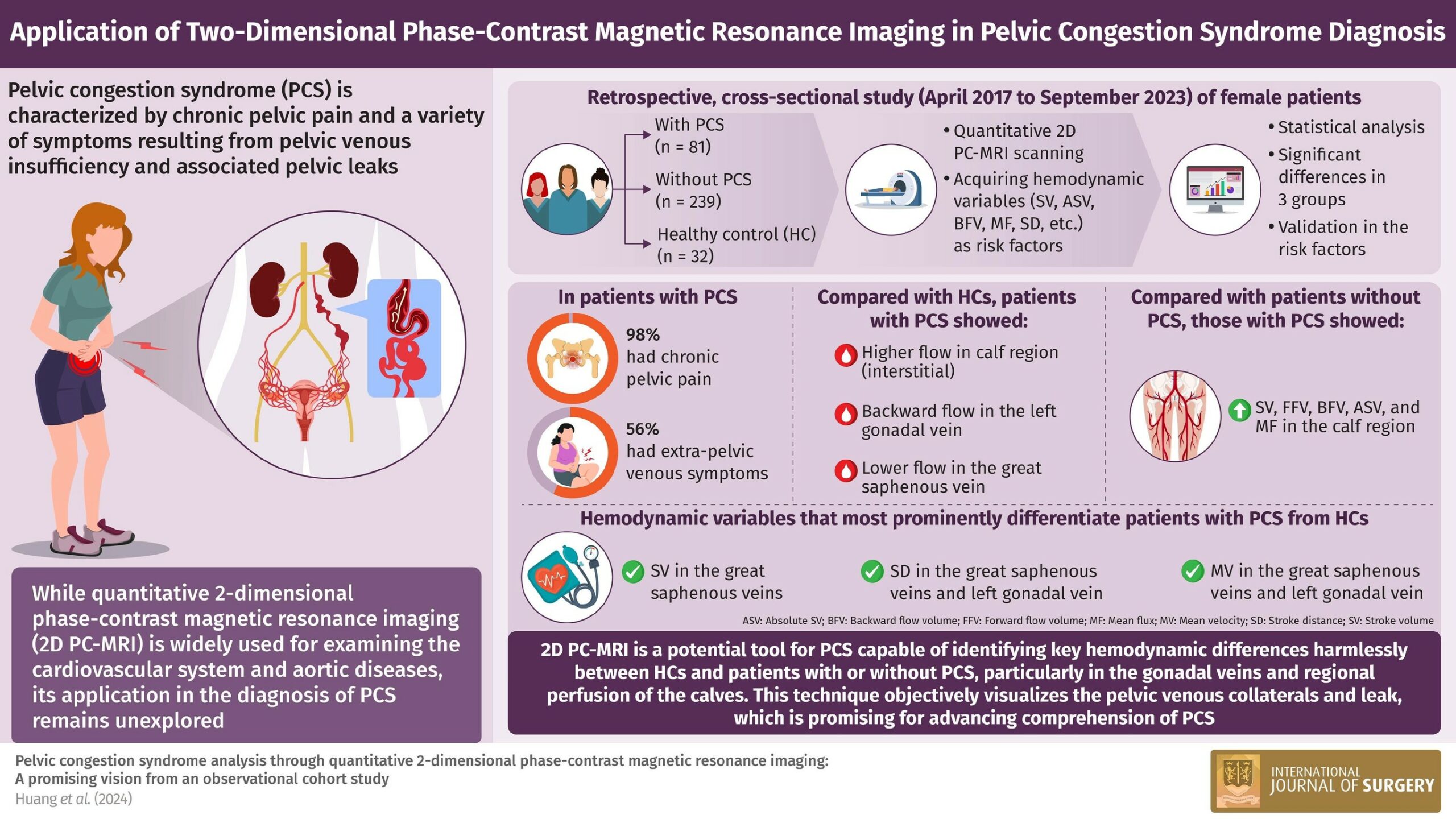
If chronic pelvic pain persists despite treatment, it’s also important to consider Pelvic congestion syndrome, a condition that is less commonly discussed.
In such cases, you may want to consult a vascular specialist, such as Dr. Huang, for further evaluation and management.
How Long Does PID Last? See a Specialist for Proper Care
Recovery time for pelvic inflammation varies from person to person. If the infection is mild and treated promptly, most people recover within one to two weeks.
However, delayed treatment or more severe infections may require longer recovery periods and carry a higher risk of complications.
If you experience symptoms such as abdominal pain, fever, or abnormal bleeding, early diagnosis and treatment are highly recommended.
If you suspect pelvic congestion or inflammation-related pelvic pain, feel free to consult Dr. Huang’s cardiovascular surgery clinic for expert evaluation and care.
Get Expert Cardiovascular Advice Now
Expert Surgeons for Comprehensive Cardiovascular Treatment!
Instant Online Consultation Available